Meta analysis of the glycemic outcomes with the use of the Conversation Map tools to deliver diabetes self-management education and support (DSME/S)
August 31, 2016
August 31, 2016 — by Barbara Eichorst, MS, RD, CDE Vice President of Clinical Practice, Healthy Interactions, and Rachel Raia, MPH, CPHQ Data and Research Consultant, Healthy Interactions
Introduction
Healthy Interactions’ Conversation Map tools are the most deployed DSME/S curriculum in the world. The diabetes Map tools were developed in collaboration with the American Diabetes Association in the U.S.A. and the International Diabetes Federation outside of the USA. Over 80,000 diabetes educators have been trained to facilitate the Map sessions in over 120 countries. The effectiveness of the Map tools can vary from one cohort to the next due to cultural implications, although the program has been translated and made culturally relevant for each country in which it is used. Previous research assessing outcomes for specific cohorts of patients has been collected, but this is the first study to evaluate Map tools outcomes at the macro level.
Purpose
To evaluate the outcomes of Conversation Map tools from a larger, more diverse sample size, representing patients from many countries and cultures, as measured by change in HbA1c.
Objective
Conduct a meta-analysis to evaluate glycemic outcomes using Conversation Map tools to deliver diabetes self-management education and support (DSME/S).
Subjects
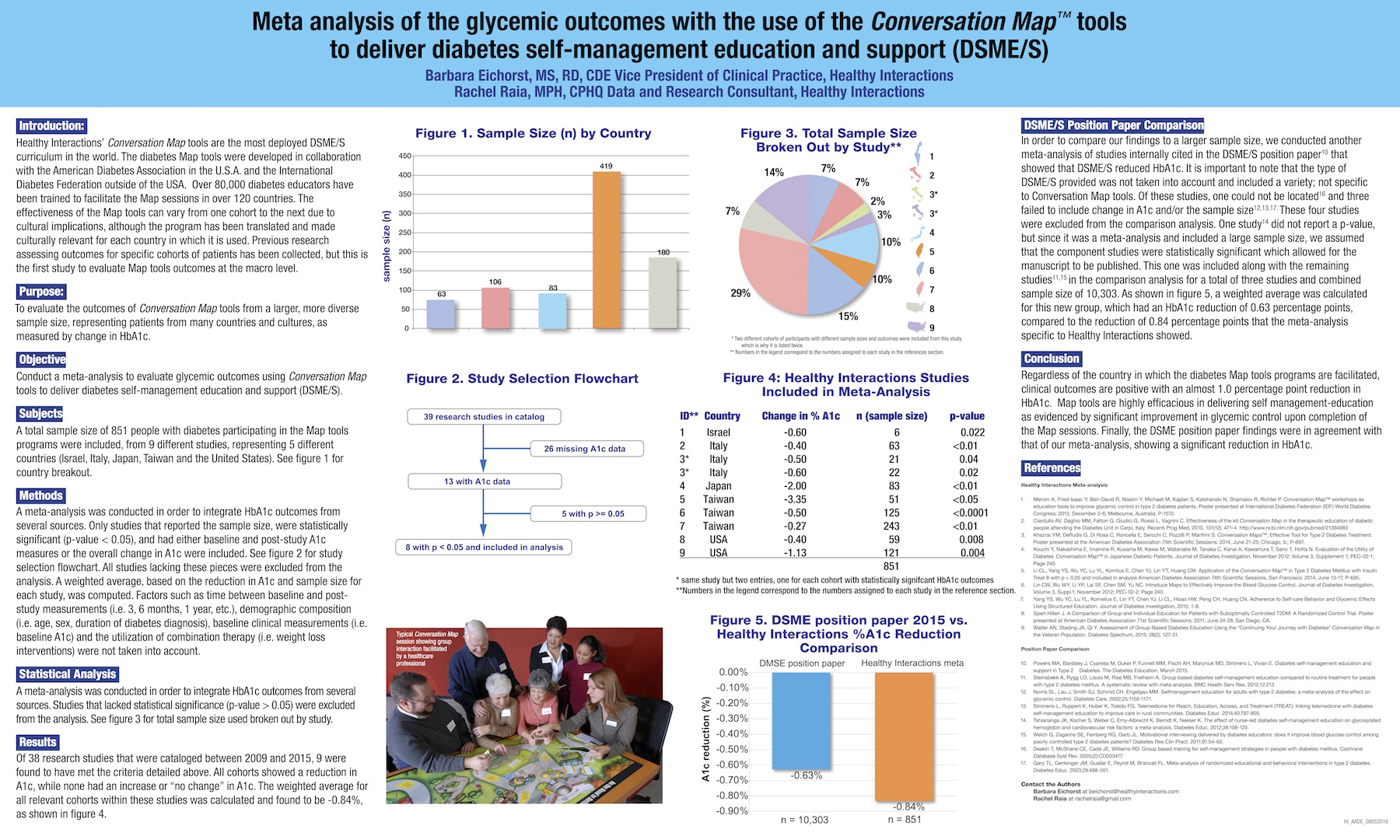
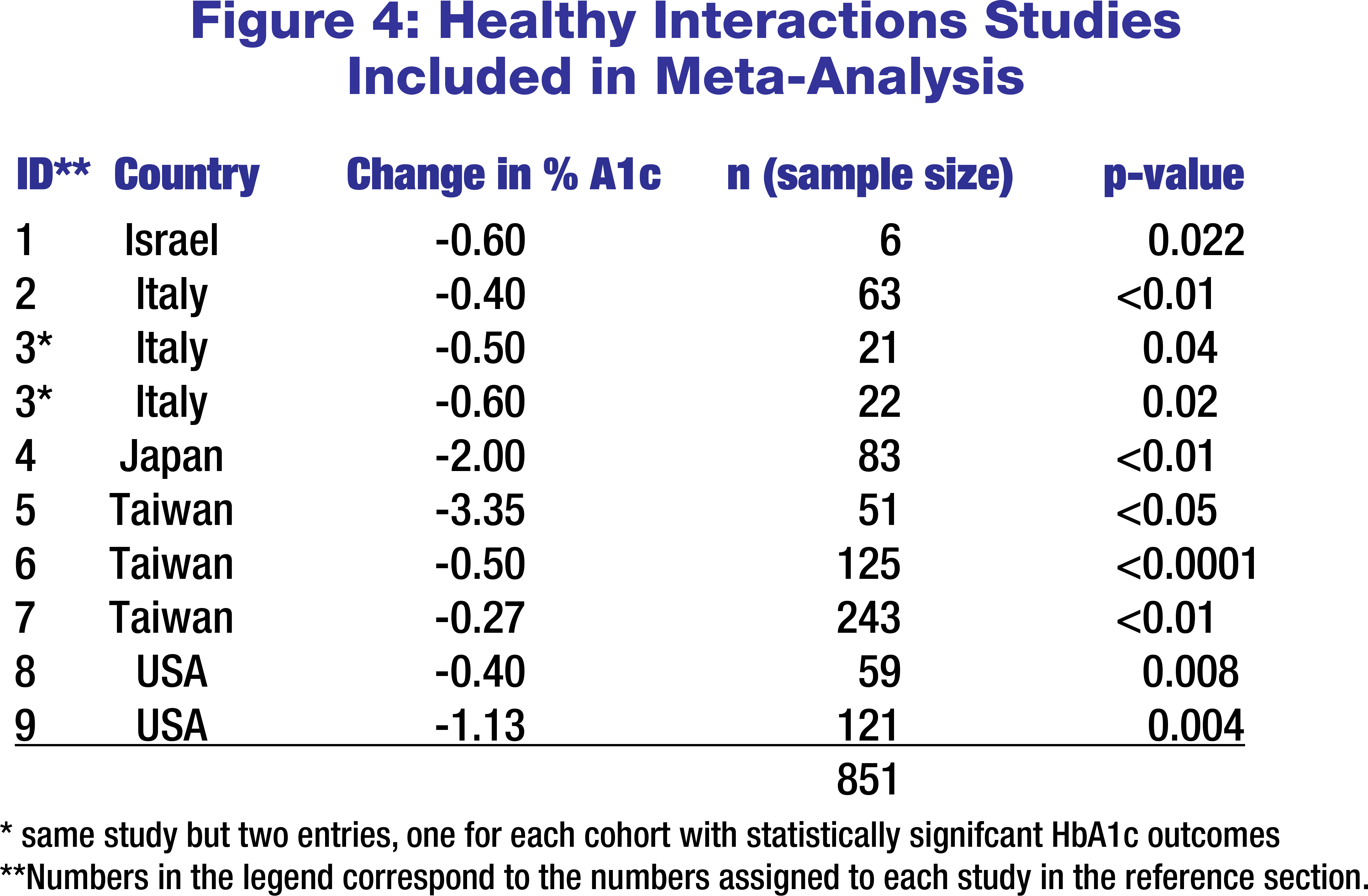
A total sample size of 851 people with diabetes participating in the Map tools programs were included, from 9 different studies, representing 5 different countries (Israel, Italy, Japan, Taiwan and the United States). See figure 1 for country breakout.
Methods
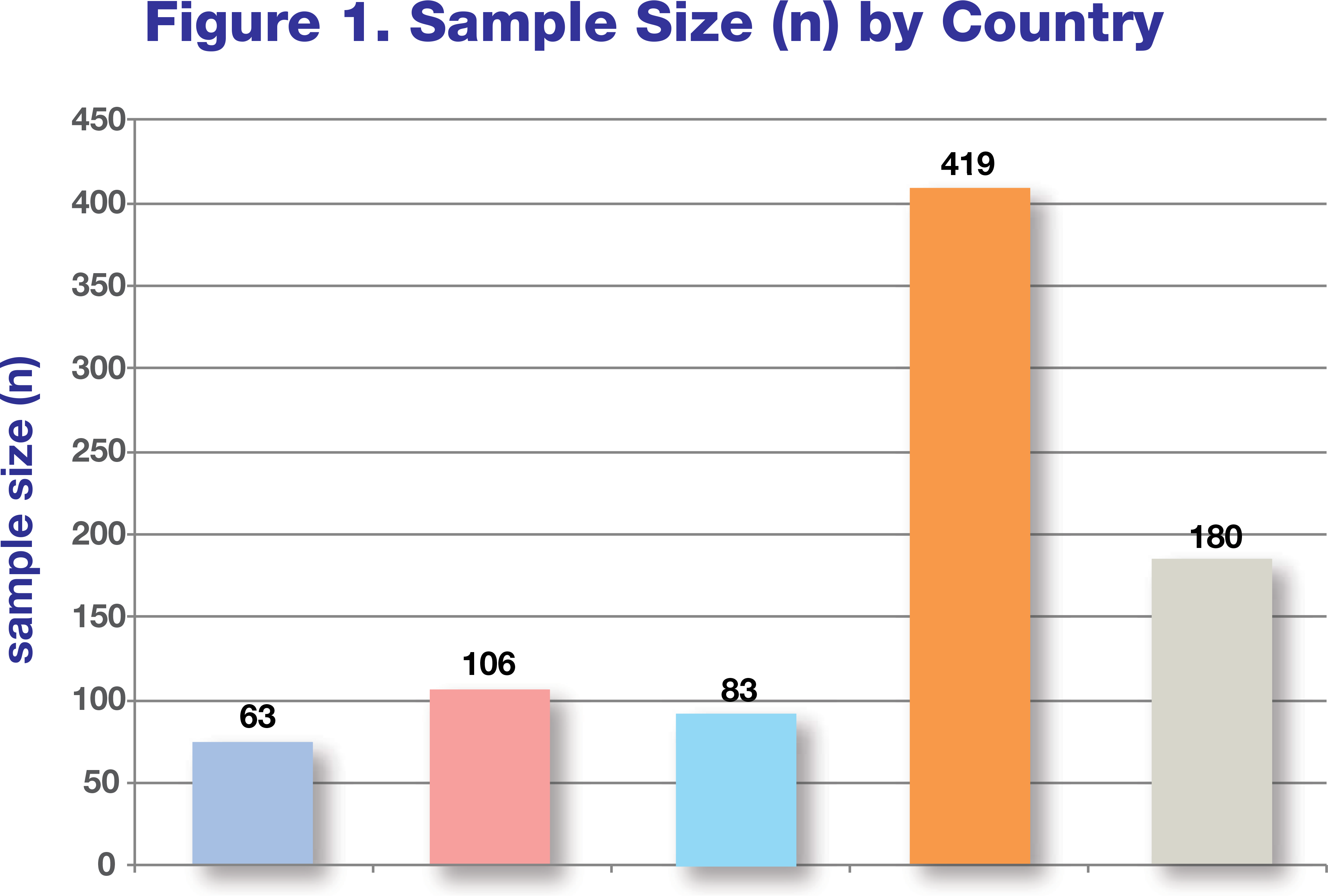
A meta-analysis was conducted in order to integrate HbA1c outcomes from several sources. Only studies that reported the sample size, were statistically significant (p-value < 0.05), and had either baseline and post-study A1c measures or the overall change in A1c were included. See figure 2 for study selection flowchart. All studies lacking these pieces were excluded from the analysis. A weighted average, based on the reduction in A1c and sample size for each study, was computed. Factors such as time between baseline and post- study measurements (i.e. 3, 6 months, 1 year, etc.), demographic composition (i.e. age, sex, duration of diabetes diagnosis), baseline clinical measurements (i.e. baseline A1c) and the utilization of combination therapy (i.e. weight loss interventions) were not taken into account.
Statistical Analysis
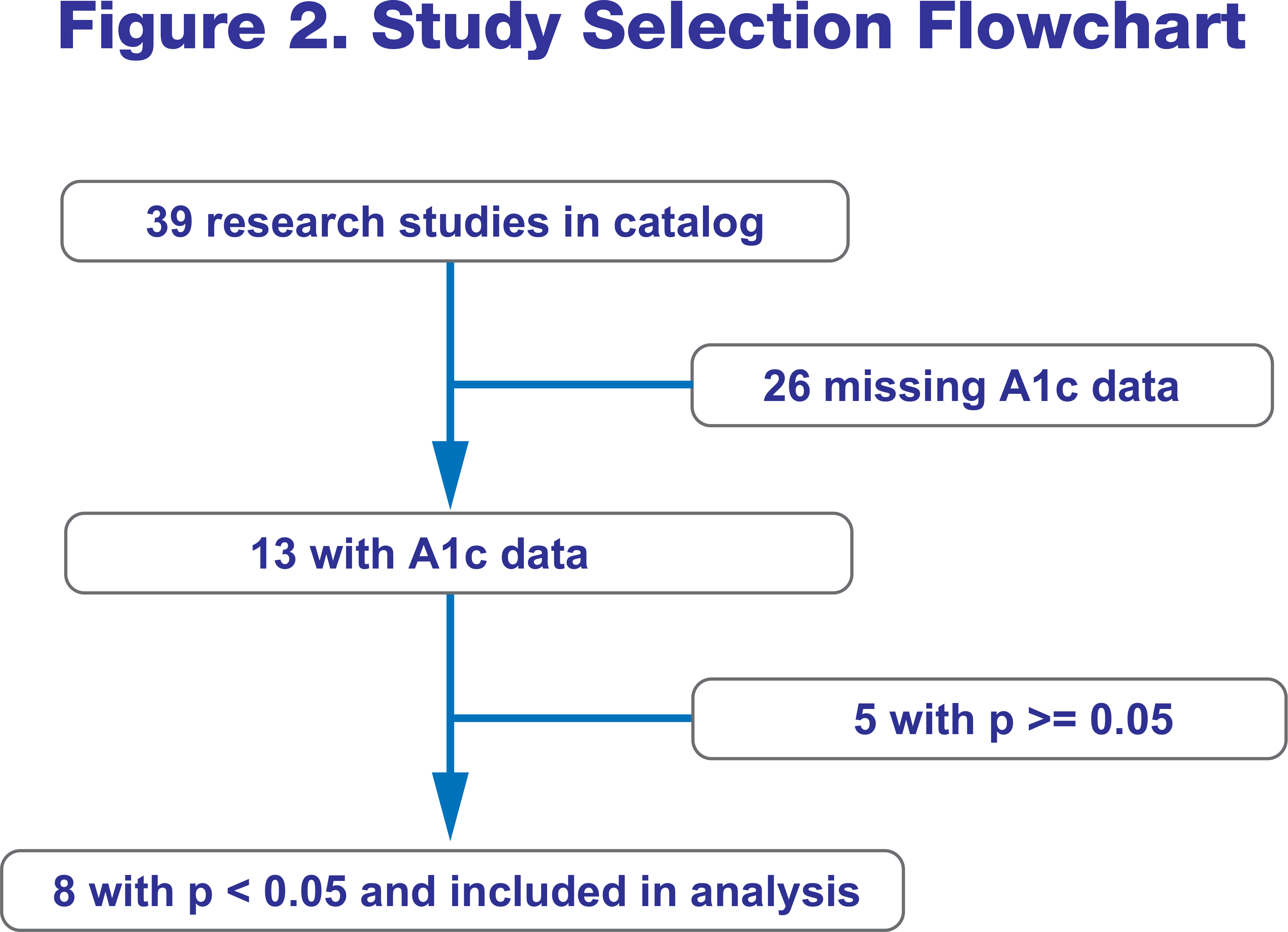
A meta-analysis was conducted in order to integrate HbA1c outcomes from several sources. Studies that lacked statistical significance (p-value > 0.05) were excluded from the analysis. See figure 3 for total sample size used broken out by study.
Results
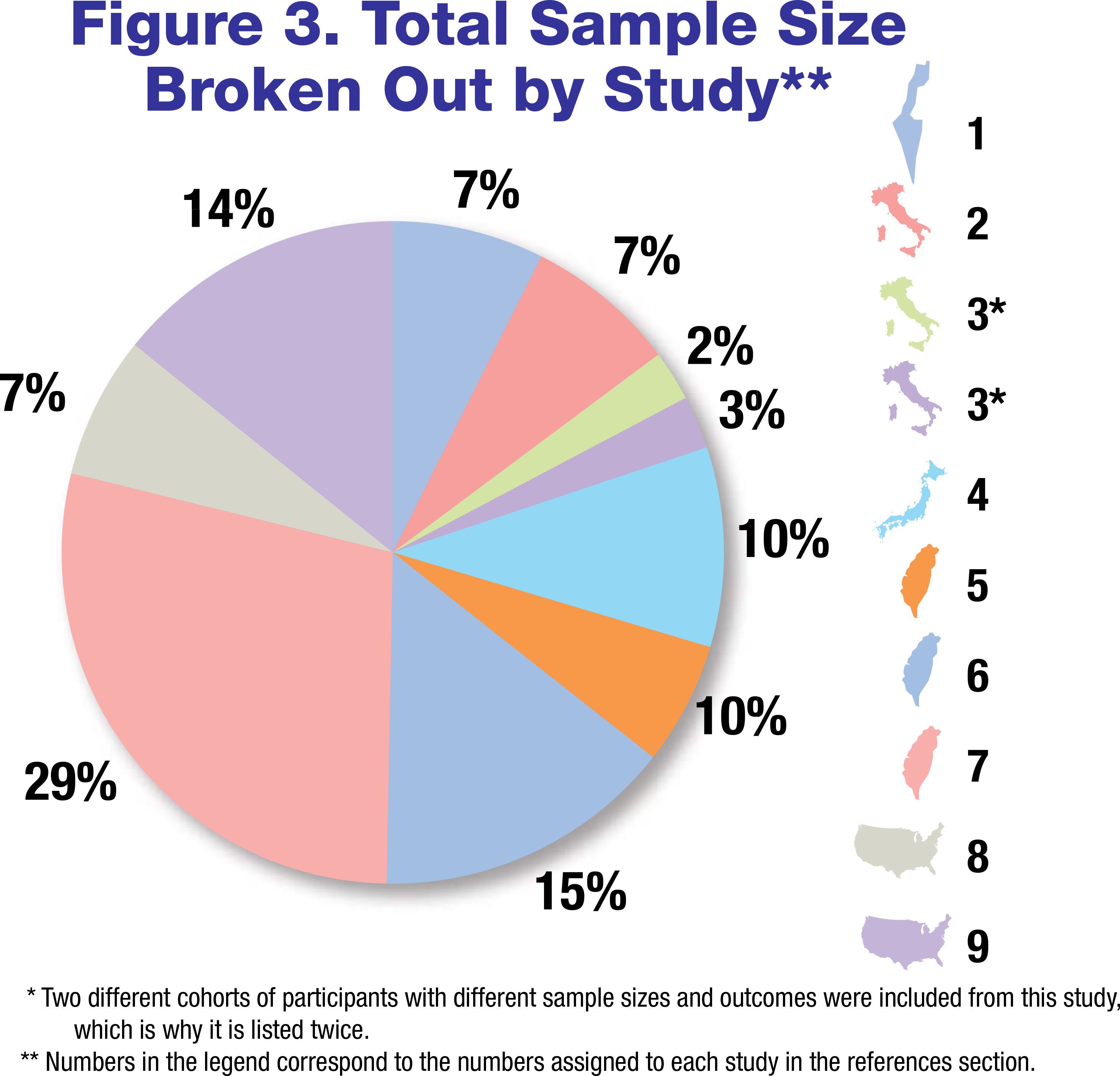
Of 38 research studies that were cataloged between 2009 and 2015, 9 were found to have met the criteria detailed above. All cohorts showed a reduction in A1c, while none had an increase or “no change” in A1c. The weighted average for all relevant cohorts within these studies was calculated and found to be -0.84%, as shown in figure 4.
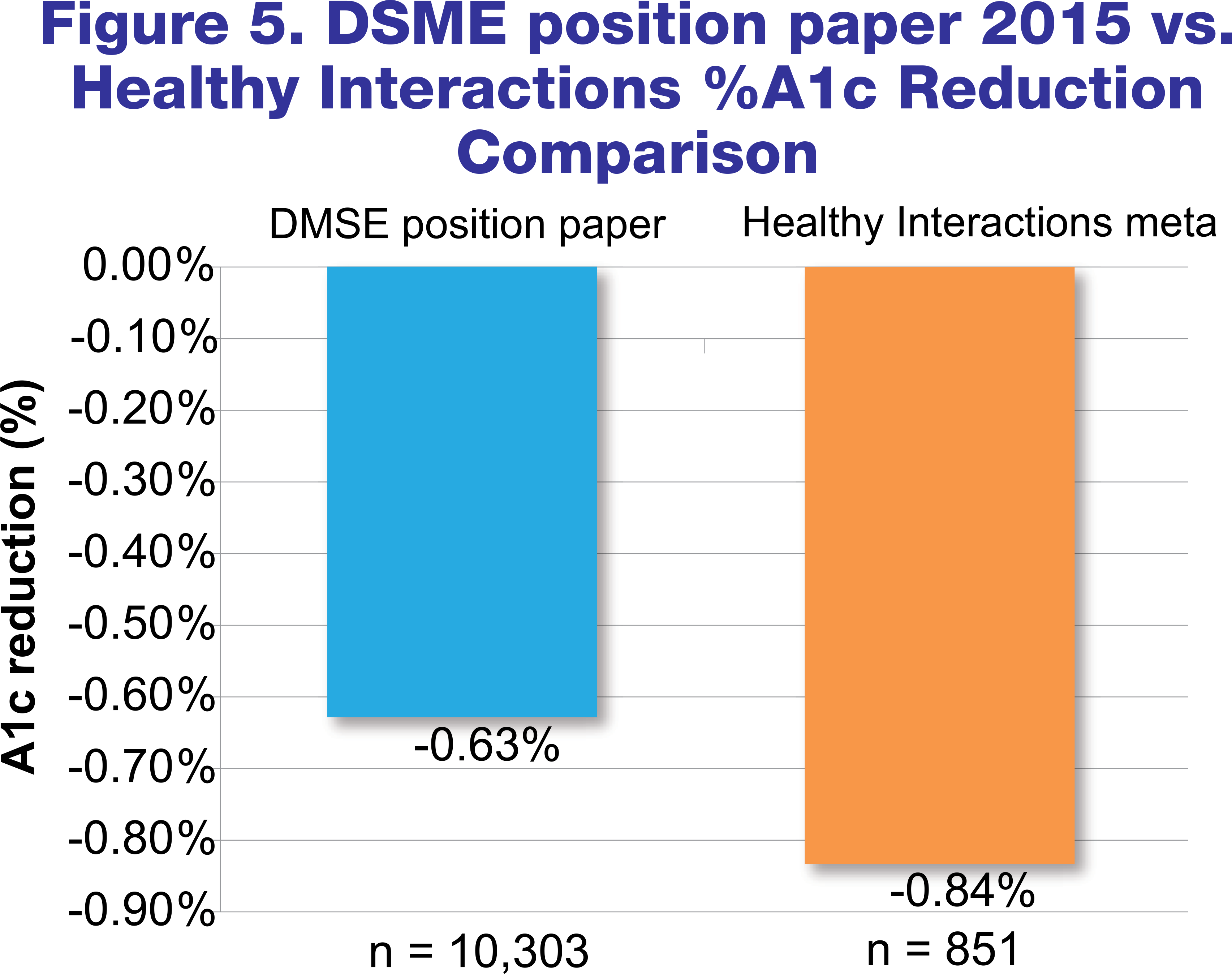
DSME/S Position Paper Comparison
In order to compare our findings to a larger sample size, we conducted another meta-analysis of studies internally cited in the DSME/S position paper10 that showed that DSME/S reduced HbA1c. It is important to note that the type of DSME/S provided was not taken into account and included a variety; not specific to Conversation Map tools. Of these studies, one could not be located16 and three failed to include change in A1c and/or the sample size12,13,17. These four studies were excluded from the comparison analysis. One study14 did not report a p-value, but since it was a meta-analysis and included a large sample size, we assumed that the component studies were statistically significant which allowed for the manuscript to be published. This one was included along with the remaining studies11,15 in the comparison analysis for a total of three studies and combined sample size of 10,303. As shown in figure 5, a weighted average was calculated for this new group, which had an HbA1c reduction of 0.63 percentage points, compared to the reduction of 0.84 percentage points that the meta-analysis specific to Healthy Interactions showed.
Conclusion
Regardless of the country in which the diabetes Map tools programs are facilitated, clinical outcomes are positive with an almost 1.0 percentage point reduction in HbA1c. Map tools are highly efficacious in delivering self management-education as evidenced by significant improvement in glycemic control upon completion of the Map sessions. Finally, the DSME position paper findings were in agreement with that of our meta-analysis, showing a significant reduction in HbA1c.
References
Healthy Interactions Meta-analysis
1 Merom A, Fried Isaac Y, Ben-David R, Nissim Y, Michaeli M, Kaplan S, Katshanski N, Shamalov R, Richter P. Conversation MapTM workshops as education tools to improve glycemic control in type 2 diabetes patients. Poster presented at International Diabetes Federation (IDF) World Diabetes Congress: 2013, December 2-6; Melbourne, Australia; P-1572.
2 Ciardullo AV, Daghio MM, Fattori G, Giudici G, Rossii L, Vagnini C. Effectiveness of the kit Conversation Map in the therapeutic education of diabetic people attending the Diabetes Unit in Carpi, Italy. Recenti Prog Med, 2010, 101(12): 471-4. http://www.ncbi.nlm.nih.gov/pubmed/21394983
3 Khazrai YM, Deffudis G, Di Rosa C, Roncella E, Sercchi C, Pozzilli P, Manfrini S. Conversation MapsTM, Effective Tool for Type 2 Diabetes Treatment. Poster presented at the American Diabetes Association 75th Scientific Sessions: 2014, June 21-25; Chicago, IL; P-697.
4 Kouchi Y, Nakashima E, Imamine R, Kusama M, Kawai M, Watanabe M, Tanaka C, Kanai A, Kawamura T, Sano T, Hotta N. Evaluation of the Utility of Diabetes Conversation MapTM in Japanese Diabetic Patients. Journal of Diabetes Investigation, November 2012; Volume 3, Supplement 1; PEC-02-1; Page 240.
5 Li CL, Yang YS, Wu YC, Lu YL, Kornlius E, Chen YJ, Lin YT, Huang CM. Application of the Conversation MapTM in Type 2 Diabetes Mellitus with Insulin Treat 8 with p < 0.05 and included in analysis American Diabetes Association 74th Scientific Sessions, San Francisco: 2014, June 13-17, P-695.
6 Lin CW, Wu WY, Li YP, Lai SF, Chen SM, Yu NC. Introduce Maps to Effectively Improve the Blood Glucose Control. Journal of Diabetes Investigation, Volume 3, Suppl.1; November 2012; PEC-02-2; Page 240.
7 Yang YS, Wu YC, Lu YL, Kornelius E, Lin YT, Chen YJ, Li CL, Hsiao HW, Peng CH, Huang CN. Adherence to Self-care Behavior and Glycemic Effects Using Structured Education. Journal of Diabetes investigation, 2015; 1-8.
8 Sperl-Hillen J. A Comparison of Group and Individual Education for Patients with Suboptimally Controlled T2DM: A Randomized Control Trial. Poster presented at American Diabetes Association 71st Scientific Sessions: 2011, June 24-28; San Diego, CA.
9 Walter AN, Stading JA, Qi Y. Assessment of Group-Based Diabetes Education Using the "Continuing Your Journey with Diabetes" Conversation Map in the Veteran Population. Diabetes Spectrum, 2015; 28(2), 127-31.
Position Paper Comparison
10 Powers MA, Bardsley J, Cypress M, Duker P, Funnell MM, Fischl AH, Maryniuk MD, SIminero L, Vivian E. Diabetes self-management education and support in Type 2 Diabetes. The Diabetes Education, March 2015.
11 Steinsbekk A, Rygg LO, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12:213
12 Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Selfmanagement education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159-1171.
13 Siminerio L, Ruppert K, Huber K, Toledo FG. Telemedicine for Reach, Education, Access, and Treatment (TREAT): linking telemedicine with diabetes self-management education to improve care in rural communities. Diabetes Educ. 2014;40:797-805.
14 Tshiananga JK, Kocher S, Weber C, Erny-Albrecht K, Berndt K, Neeser K. The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ. 2012;38:108-123.
15 Welch G, Zagarins SE, Feinberg RG, Garb JL. Motivational interviewing delivered by diabetes educators: does it improve blood glucose control among poorly controlled type 2 diabetes patients? Diabetes Res Clin Pract. 2011;91:54-60.
16 Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003417.
17 Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003;29:488-501.
Other recent news
September 2, 2015
October 17, 2015
July 27, 2015
July 23, 2015
March 23, 2015