HEALTHY CONNECTIONS: April 2016

Welcome to the April edition of Healthy Connections. This month’s newsletter highlights Personal Health Engagement™, the health engagement process, and the ways that it can be measured. We also look at an updated Joint Position Statement from the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics, while focusing on the statement’s updated evidence regarding diabetes self-management education and support (DSME/S).
Healthy Connections has been organized into two quick read sections:

 Personal Health Engagement™ (PHE) is the continuum of individual involvement and empowerment in health and wellness. The health engagement process is intended to generate self-fulfillment in daily living and ultimately improve quality of life and health outcomes.
Personal Health Engagement™ (PHE) is the continuum of individual involvement and empowerment in health and wellness. The health engagement process is intended to generate self-fulfillment in daily living and ultimately improve quality of life and health outcomes.
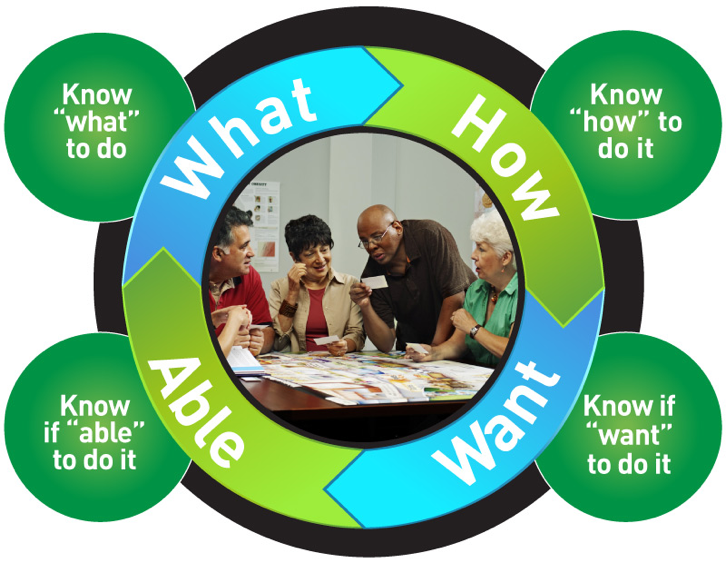
The PHE process starts with effective communication between an individual and his or her health care providers. A productive exchange of ideas and strategies leads to personal accountability and involvement in decision-making that is followed by improvement in clinical care outcomes. PHE can be measured by:
- Health ownership: a person's belief in his own competence in self-care management. Health status perceptions and health belief systems impact the level of responsibility for self-care.
- Behavior change motivation: a level of being ready and willing to change certain behaviors in order to improve health status. It is also an attitude towards change and related emotions.
- Actionable: being prepared to act on self-managements tasks. Determining the specific actions and ability to implement short and long-term goals of self-care management.
- Utilize support network: the ability to solicit support from HCPs, peers and family.
- Knowledgeable: the level of knowledge it takes to know what to do about health related behaviors and how to go about it. The ability to assess the risk of health related repercussions.
- Resourceful: the willingness to solicit information related to self-care from various media channels.
- Adaptable/Responsive: the willingness to change actions in response to health status changes or changes in psychological or social circumstances.
Healthy Interactions’ PHE programs activate, prepare, empower, and support individuals to act on the desirable behaviors to positively influence outcomes. PHE programs are designed to simplify the process of behavior change for both the patients and the health care professionals involved. The realities of daily living are put into strategic focus, allowing an individual to embrace change and enjoy the process of making the changes in their lives.
PHE programs are inclusive in all aspects of behavior change needed to promote improvement in care. PHE helps in prioritizing on actionable behaviors like healthy eating, physical activity, taking medications, dealing with family, friends, co-workers, health care systems, and decision making for daily tasks. PHE also monitors progress in self-care, relapses, and adjusts for changes in psycho-social circumstances.
PHE methodology is designed to improve patient care outcomes, improve the delivery of care, help the patient, and help the health care professional. Appropriately trained and equipped professionals use the PHE programs either as stand alone curriculums for disease self-management or to complement existing programs.

Our first continuing education (CE) webinar for dietitians, nurses, and pharmacists, “The Diabetes Educator Role in Delivering Diabetes Self-Management Education and Support (DSME/S) in Healthcare Systems” was delivered on March 15, 2016 and showcased evidence-based diabetes self-management education and support in type 2 diabetes. In 2015, we were provided with an updated Joint Position Statement from the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics that surfaced new evidence regarding the effectiveness of DSME. We now have evidence that DSME is cost-effective, improves A1c by as much as 1%, reduces diabetes complications, improves quality of life, improves healthy eating and physical activity, increases healthy coping, enhances self-efficacy and empowerment, and decreases distress as well as depression.
The most meaningful practice driver resulting from the Joint Position Statement is the DSME and DSME/S algorithm of care that outlines the critical times to assess, provide, and adjust this effective intervention. We also have evidence that better outcomes have been shown to be associated with the amount of time spent with a diabetes educator. This is an exciting time for all of us diabetes educators as our roles are validated and opportunities to impact people with diabetes are maximized. Happy spring!


