Addressing Diabetes in Family Practice Environment: Tools Support Sustainable Behavior Change
June 13, 2016
August 18, 2016 — by David Moen, M.D., and Barbara Eichorst, M.S., R.D., CDE
Objectives:
- Leverage a behavioral change model to optimize the value of diabetes disease management.
- Deliver national standards for diabetes self-management education and support (DSME/S).
- Increase volume of patients who engage in diabetes population health management.
- Reach patients who are not engaged in self-care or are challenged by diabetes self-care.
- Ensure care providers are integrated as member of a diabetes management team;optimize value of personal interaction.
- Improve clinical outcomes for patients with diabetes.
 |
Program Description:An estimated 19 million people in the US have been diagnosed with diabetes. Nearly seven million are believed to be living with undiagnosed diabetes. Additionally, nearly 80 million people are estimated to have blood glucose levels indicative of pre- diabetes or increased risk for diabetes. Alarmingly, more than 100 million Americans are at risk for developing devastating complications from diabetes.1 The total cost of patients with diabetes who have their HbAlc levels in control is significantly less than for those without it. The percentage of people with controlled diabetes is low and eroding. Our overburdened healthcare system will continue to be taxed, and costs will continue spiraling out of control unless diabetes is better managed.DSME/S is necessary to improve outcomes. The National Standards for Diabetes Self-Management Education define quality diabetes self-management education and assist clinicians in providing evidence-based learning. Organizations seeking Medicare reimbursement for DSME/S must meet 10 national standards, which include internal structure, external input, access, program coordination, instructional staff, curriculum, individualization, ongoing support, patient progress and quality improvement.2 |
The American Diabetes Association (ADA) and the American Association of Diabetes Educators (AADE) offer recognition/accreditation to sites that meet and uphold these standards. The ADA program is called the Education Recognition Program (ERP), and AADE’s is called the Diabetes Education Accreditation Program (DEAP).3
Founded in 1975, Village Family Practice (VFP) has grown to a practice of 20 physicians providing primary care in several locations across the greater Houston area. As a member of the Accountable Care Coalition of Texas, an accountable care organization (ACO) that participates in CMS’ Medicare Shared Savings Program, VFP has a vested interest in reducing costs and improving outcomes for patients with diabetes. Six of 33 CMS-required reporting measures are specific to diabetes. Achieving goals for these measures results in financial rewards to the provider, as well as improved health among their patient populations.
In early 2014, VFP partnered with Healthy Interactions to provide a comprehensive and evidence-based DSME/S. The ERP status was approved in April of 2014, and the program was launched in November of the same year. ERP status allows VFP to get reimbursed for the DSME, as well as ensuring that the service is provided within the standards that produce optimal outcomes for all. Ultimately, the practice is able to achieve better HbA1c outcomes and provide the best in DSME/S.
Healthcare providers (HCPs) who provide DSME/S use Healthy Interactions’ Conversation Map tools® for interactive, evidence-based, chronic illness management education programs. The tools engage persons with diabetes (PWDs) in exploring their feelings, information and implications of their choices related to managing their health conditions with others in a safe, intimate environment. The sessions are supported by a digital coaching platform and app. During a Map session, PWDs are prompted to self-manage their conditions. In between Map sessions, patients are engaged in self-care management, with digital platform coaching from their healthcare provider, as well as use of the app to help achieve their short- vs. long-term goals.
Evaluation Process: Medicare requires that nine of 10 hours of DSME/S be administered via group sessions. The remaining one hour can be delivered individually, but it can also be delivered in a group setting if more appropriate. Healthy Interactions focuses mostly on group education sessions because one-on-one sessions have not proved as effective when it comes to patient program completion. Group sessions have been successful because the curriculum is totally centered on the participant and allows for individualization within a group environment. A group creates a support network, incentivizing patients to return for additional sessions.
Map tools meet program recognition/accreditation criteria for a complete DSME/S curriculum within ERP and DEAP. In the ERP program, providers can more easily add information about Map education sessions and track progress because Map tools are part of an HCPs “Chronicle,” an online system allowing for assessment, documentation and reporting in accordance with ADA standards and National Committee for Quality Assurance (NCQA) requirements.
Between sessions and after completing the program, participants use a digital application to support goals and stay up to date on diabetes self-care management. Once finished with 10 hours, patients are eligible for additional DSME/S that includes two hours as allowed by Medicare. These hours cover use of the digital platform for goal-setting and access to educational information. The app enables PWDs to connect with their HCPs.
Results
Since the initiation of the ERP status in VFP, more than 300 patients have participated in Map sessions.
About 80% of patient referrals came from two of the practice’s physician champions. One physician is part of the ERP advisory committee and firmly believes in the benefits of DSME/S. Data show that when a provider understands the value of DSME/S and is involved in its delivery, more patients are referred and engagement is more fully promoted. This increases attendance and the likelihood that patients will complete a full program.
VFP offered a total of 147 sessions between February 2014 and April 2016. Just under a third of patients completed all 10 hours of DSME. Data reflect an increase in the confidence of patients to provide self-care. In addition, more than 95% of participants indicated a desire to attend additional sessions.
Perhaps most importantly, the program produced clinical outcome improvement in glycemic control of 11%. This means that PWDs are improving their HbA1c levels and the program delivers on its mission.
Subsequent to implementing the program at VFP, outcomes were evaluated for the time period of 2014 and 2015. A random sample of 60 patients with diabetes (30 completing the Map tools program and 30 who did not engage with the program) was evaluated. With similar baseline A1c measurements between the groups, the average reduction in A1c for the intervention group was more than four times that of the control group. The intervention group also had a greater number of participants who had a decrease in their A1c, and fewer who had an increase.
Lessons Learned
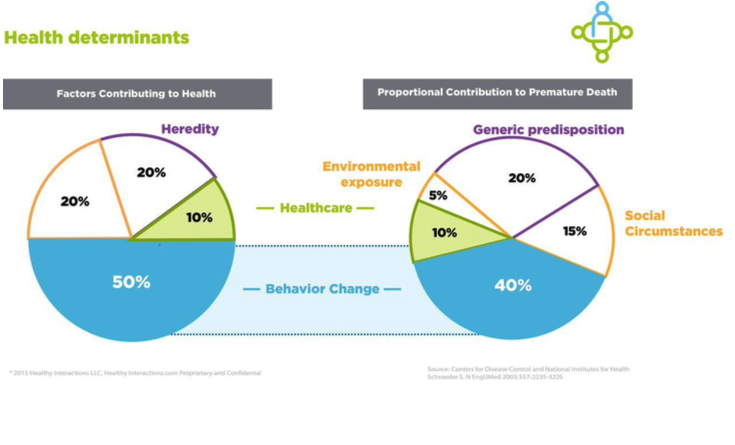
- We know from innumerable studies that behavior change spells the difference between success and failure.
- This case study shows the sustained effectiveness of patient engagement in group settings when a group is led by a healthcare provider trained in using Conversation Map methodology along with digital support.
|
 |
As trusted HCPs, nurses, dietitians, pharmacists and doctors have unique opportunities to invite PWDs to engage. DSME/S, if provided within its intended scope, improves outcomes for PWDs.4 However, only 6.8% of individuals newly diagnosed with type 2 diabetes that have private insurance received DSME/S in the first year of diagnosis,5 and 4% of people with Medicare received DSME.6 With this rate, health systems are not very likely to achieve the Healthy People 2020 goal that calls for a target of 56.8% to 62.5%.7 The Conversation Map uniquely increases access to DSME/S while also optimizing quality and outcomes.
- VFP is now focused on increasing DSME/S referrals and empowering its providers to engage in patient-focused diabetes conversations. Digital DSME/S will continue to be valuable for increasing engagement and program completion rate.
- A yet-to-be-solved challenge is identifying patients who are most in need of an intervention by using clinical decision support systems that embed evidence-based appropriateness criteria. Healthy Interactions is developing this type of end-to-end system and is integrating it into an electronic health record. This system will powerfully identify the most at-risk patients, send messages inviting them to group sessions and alert physicians to prescribe DSME/S.
- To support triple aim success, the system incorporates analytics capabilities that review physician ordering and patient compliance. Reports help organizations understand what is needed to ensure they are reaching outcome benchmarks, such as A1c scores.
- One patient shared this comment: “Not as terrifying as other people may believe. I attended a class years ago about ‘count this and count that, do this and don't do that.’ I never stuck to it. This is way better. I like your way.”
- Patient-reported outcomes and satisfaction were high. When asked what was most meaningful about the Conversation Map session, responses included:
- Understanding my meds and tracking.
- Relating to others’ opinions and comments.
- Discussion about symptoms and experiences.
- Signs of high/low blood glucose.
- Learning about my insulin and educating myself.
- Good information and goal setting.
1 “National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011.” Centers for Disease Control and Prevention. U.S. Department of Health and Human Services. 2011.
2 Haas L, Maryniuk M, Beck J, Cox CE, et al. “National Standards for Diabetes Self-Management Education and Support.” Diabetes Care. November 2012;35(11):2393-2401.
3 Powers M, Bardsley J, et al. “Diabetes Self-Management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators and the Academy of Nutrition and Dietetics.” Diabetes Care. June 5, 2015;38:1–11.
4 Ibid.
5 Li R, Shrestha SS, Lipman R, Burrows NR, et al. “Diabetes Self-Management Education and Training Among Privately Insured Persons With Newly Diagnosed Diabetes—United States, 2011-2012.” Morbidity and Mortality Weekly Report. Nov. 21, 2014;63(46):1045-1049.
6 Duncan I, Birkmeyer C, Coughlin S, Li Q, Sherr D, Boren S. “Assessing the Value of Diabetes Education.” Diabetes Education. September-October 2009;35(5):752–760.
7 ”Healthy People 2020: Diabetes Overview.” Office of Disease Prevention and Health Promotion. Healthypeople.gov.
David Moen, M.D., is chief medical officer, and Barbara Eichorst, M.S., R.D., CDE, is vice president, clinical, both at Healthy Interactions.
Other recent news
September 2, 2015
October 17, 2015
July 27, 2015
July 23, 2015
March 23, 2015
